Plantar fasciitis is one of the most common causes of heel pain, affecting millions of people each year. This condition occurs when the plantar fascia—a thick band of tissue that runs along the bottom of your foot connecting your heel bone to your toes—becomes inflamed or irritated. Understanding what plantar fasciitis is, what may contribute to it, and the various approaches people use to find relief can help you make informed decisions about your foot health.
What Is Plantar Fasciitis?
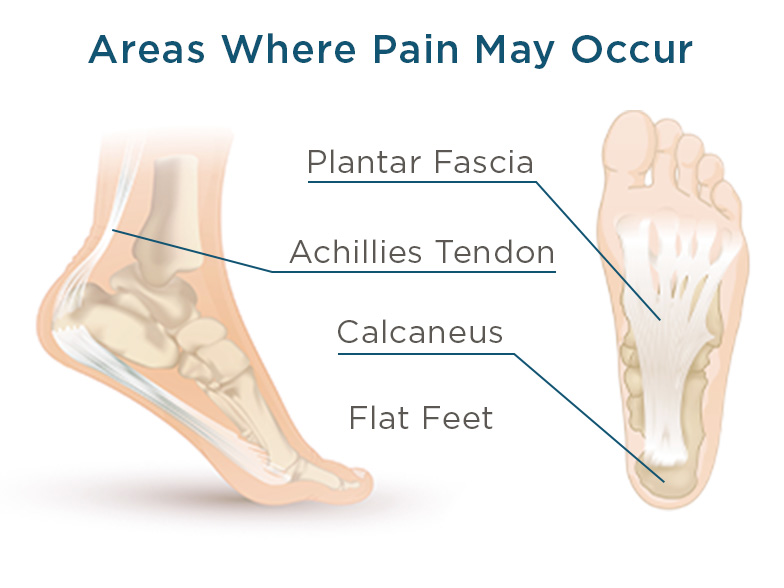
The plantar fascia acts as a shock absorber and supports the arch of your foot. When this tissue experiences excessive stress or strain, small tears can develop, leading to inflammation and the characteristic heel pain associated with plantar fasciitis. The condition is also sometimes referred to as plantar fascia pain or heel pain plantar fasciitis.
Many people describe the pain as a stabbing sensation in the bottom of the foot near the heel. This discomfort is often most noticeable with the first steps in the morning or after periods of rest, though it can also occur after standing or walking for extended periods.
What Causes Plantar Fasciitis?
Understanding the causes of plantar fasciitis can help you identify potential risk factors. While anyone can develop this condition, certain factors may increase the likelihood:
Common Risk Factors
Age and Activity Level: Plantar fasciitis is most common in people between ages 40 and 60. Runners, dancers, and people whose activities place significant stress on their feet may be at higher risk.
Foot Mechanics: Certain foot structures can contribute to plantar fasciitis development. People with flat feet, high arches, or abnormal walking patterns may experience increased stress on the plantar fascia. The way you walk can affect how weight is distributed across your foot.
Weight: Carrying excess weight puts additional pressure on the plantar fascia with each step.
Occupational Factors: Jobs that require long hours of standing or walking on hard surfaces—such as factory workers, teachers, or retail employees—may increase strain on the feet.
Inadequate Footwear: Shoes with poor arch support, thin soles, or worn-out cushioning don't properly support the foot's natural structure. This is why choosing appropriate footwear is so important for foot health.
Tight Calf Muscles: Limited flexibility in the calf muscles can affect your ability to flex your foot, which may place additional stress on the plantar fascia.
Plantar Fasciitis Symptoms
Recognizing the symptoms of plantar fasciitis can help you understand whether you might be dealing with this condition. Common signs include:
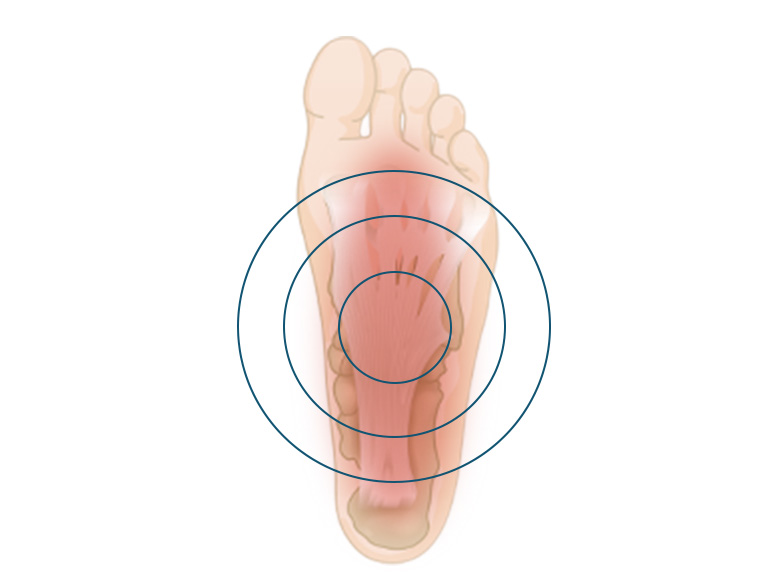
Where Is Plantar Fasciitis Pain Located?
The most common location for plantar fasciitis pain is the bottom of the foot, near the heel. Some people experience pain in the arch of the foot as well. The discomfort typically affects one foot, though it can occur in both feet simultaneously.
Common Symptom Patterns
Morning Pain: Many people notice sharp, stabbing pain with their first steps after waking up. This occurs because the plantar fascia tightens during rest and stretches suddenly when you stand.
Pain After Rest: Similar to morning discomfort, pain often occurs after sitting for extended periods, improving as you move around.
Post-Activity Discomfort: While you might not feel pain during exercise or activity, discomfort often appears afterward.

Heel Pain
One of the most common plantar fasciitis symptoms is pain in the heel of your foot. This is where the plantar fascia begins, so any extra stress on your heel can cause the tissues to become inflamed. Most people feel a sharp or stabbing pain in their heel, often worse in the morning or when stepping on it after a period of inactivity.
If you’re wondering, “Why does my heel hurt?” this might be why:
- You’ve been running, walking, or jumping on hard surfaces. People who play sports where there is a lot of pounding, either on a court, across pavement, or in a gym, are more prone to heel pain.
- You have weakened muscles in the foot, typically due to getting older, when your muscles lose strength over time.
- There is excess pressure on the heel, sometimes due to weight gain.
- You’ve got tight calf muscles, which can strain your ankle, heel bone, and plantar fascia.

Arch of Foot Pain
Do you feel a tightness, achiness, or stiffness in the arch of your foot? If so, it’s likely you have plantar fasciitis. Foot arch pain stems from overstretching the plantar fascia, a common occurrence if you:
- Overpronate or supinate, meaning that your feet roll inward or outward when you walk or run.
- Have flat feet or a high arch.
- Don’t stretch your feet, ankles, or calves before exercising.
- Frequently walk barefoot or wear shoes without arch support.
- Spend a lot of time walking or standing on hard surfaces.
- Increase your activity level suddenly.
Stiffness at the Bottom of Your Foot
Sometimes the bottom of your foot might feel tight, where moving your toes up or down is difficult or your foot is just generally inflexible. If the stiffness seems to be coming from your arch or even back toward your heel, plantar fasciitis is probably the culprit. When the plantar fascia isn’t stretched or strengthened properly, certain activities, like running, walking, or standing for long periods, can irritate it, causing that uncomfortable tension and achiness in the bottom of your foot.

Swelling Around the Heel
Swelling on the bottom of your foot around your heel, along with heel pain, are symptoms of plantar fasciitis. High-impact activities, weakened foot muscles, and tight calf muscles can all put too much stress on the plantar fascia, which can, in turn, become overstretched or inflamed. It’s important to remember that with plantar fasciitis, you shouldn’t experience foot swelling alone; it’s almost always accompanied by pain in or near the heel. Consult with your doctor to ensure that the inflammation around your heel isn’t due to another condition.

A Tight Achilles Tendon
Your Achilles tendon facilitates many of the activities you enjoy every day by connecting your heel to your calf muscles to help you move. With overuse or extended use, this tendon can become tight or even painful, and you’ll typically feel it at the back of your ankle or lower leg.
While technically a separate issue from plantar fasciitis, a tight Achilles tendon is a risk factor that can lead to plantar fasciitis. Why? The body is made up of a series of connections—when one tendon or muscle is strained, other parts of your body may overcompensate. So a lack of mobility in your ankle or calf from a tight Achilles tendon can put more strain on the plantar fascia tissues in the foot, leading to heel or arch pain.
Does Plantar Fasciitis Cause Swelling?
While plantar fasciitis primarily causes pain, some people may experience mild swelling in the heel area. However, significant swelling is less common with plantar fasciitis. If you notice considerable swelling, redness, or warmth in your foot, it's important to consult with a healthcare provider to rule out other conditions.
How to Treat Plantar Fasciitis
Many people find relief from plantar fasciitis through conservative approaches. While we don't provide medical advice, we can share common strategies that people use to manage discomfort. Always consult with a healthcare professional for personalized recommendations.
Home Care Approaches
Rest and Activity Modification: Reducing activities that aggravate foot pain can give the plantar fascia time to recover. This doesn't mean complete inactivity, but rather avoiding activities that cause significant discomfort.
Ice Application: Many people apply ice to the painful area for 15-20 minutes several times daily, particularly after activities that stress the feet.
Gentle Stretching: Regular stretching of the calf muscles and plantar fascia can help improve flexibility. Some people find relief through simple stretches performed throughout the day.
Supportive Products
Arch Supports and Orthotics: One of the most popular approaches for managing plantar fasciitis involves using arch supports or orthotic inserts. These products help distribute pressure more evenly across the foot and provide support to the arch. Many people find that proper arch support for plantar fasciitis significantly improves their comfort level. Learn more about what an arch support insert needs to effectively reduce plantar fasciitis pain.
Shoe Inserts for Plantar Fasciitis: Various types of inserts are available, from over-the-counter options to custom orthotics. The best shoe inserts for plantar fasciitis typically provide cushioning, arch support, and shock absorption. Look for inserts specifically designed to support the plantar fascia and reduce strain on this tissue. Quality arch support solutions should offer proper biomechanical support tailored to your foot's needs.
Proper Footwear: Choosing the right shoes can make a significant difference. The best shoes for plantar fasciitis generally feature:
- Strong arch support
- Cushioned soles with good shock absorption
- A slightly elevated heel (but not too high)
- Firm heel counters for stability
- Adequate room in the toe box
Whether you're looking for athletic shoes, casual footwear, or even heels for plantar fasciitis, prioritizing support and cushioning is key. Some people find that shoes with built-in arch support provide better comfort than flat, unsupportive footwear.
Professional Care Options
While many people manage plantar fasciitis with home care and supportive products, others may benefit from professional treatment. Healthcare providers can offer additional options such as physical therapy, night splints, specialized stretching programs, or other interventions tailored to individual needs.
If you're looking for personalized arch support solutions, visiting a specialist who can assess your specific foot structure and needs can be valuable. Find a Good Feet location near you to explore customized support options.
Exercises and Stretches for Plantar Fasciitis
Gentle stretching and strengthening exercises are commonly recommended for people dealing with plantar fasciitis. These movements can help improve flexibility in the calf muscles and plantar fascia, potentially reducing strain and discomfort.
Calf Stretches
Tight calf muscles can contribute to plantar fasciitis, so stretching this area is often beneficial. A simple calf stretch involves standing facing a wall with one foot forward and one back, keeping the back heel on the ground while leaning into the wall.
Plantar Fascia Stretch
To directly stretch the plantar fascia, many people sit and pull their toes back toward their shin while keeping the knee straight. This stretch can be particularly helpful first thing in the morning.
Towel Stretch
Another popular stretch involves sitting with legs extended, placing a towel around the ball of your foot, and gently pulling the towel toward you while keeping your knee straight.
Strengthening Exercises
Simple exercises like picking up small objects with your toes or practicing towel scrunches (placing a towel on the floor and using your toes to scrunch it toward you) can help strengthen the muscles that support the arch.
Important Note: If any stretch or exercise causes sharp pain or significant discomfort, stop and consult with a healthcare provider. Gentle stretching should not be painful.
How to Prevent Plantar Fasciitis
While not all cases of plantar fasciitis can be prevented, certain practices may help reduce your risk:
Maintain a Healthy Weight: Reducing excess weight decreases the stress placed on your feet with each step.
Choose Supportive Footwear: Replace worn-out shoes regularly and select footwear with good arch support and cushioning. Avoid walking barefoot on hard surfaces for extended periods.
Warm Up Properly: Before engaging in physical activity, take time to stretch your calves and feet. This helps prepare the plantar fascia for the stress of exercise.
Increase Activity Gradually: When starting a new exercise program or increasing activity level, do so gradually to avoid overwhelming your feet with sudden stress.
Cross-Train: If you're a runner or engage in high-impact activities, incorporating low-impact exercises like swimming or cycling can reduce repetitive stress on your feet.
What Are the Worst Things to Do with Plantar Fasciitis?
Certain activities may aggravate plantar fasciitis and should be approached with caution:
- Going barefoot on hard surfaces
- Wearing shoes with inadequate support or thin soles
- Ignoring pain and continuing high-impact activities
- Remaining sedentary for long periods (gentle movement is generally better than complete rest)
- Wearing high heels or completely flat shoes without support
Understanding the Difference: Plantar Fasciitis vs. Other Foot Conditions
Plantar Fasciitis vs. Fallen Arches
While related, these are different conditions. Fallen arches (flat feet) refer to a foot structure where the arch has collapsed, causing the entire sole to touch the ground. Plantar fasciitis is inflammation of the plantar fascia tissue. However, people with fallen arches may be at higher risk for developing plantar fasciitis due to the altered mechanics of their feet.
Other Foot Pain Considerations
Foot pain can stem from many causes beyond plantar fasciitis. Conditions like heel spurs, stress fractures, arthritis, or nerve compression can cause similar symptoms. This is why proper evaluation by a healthcare provider is important if you're experiencing persistent foot pain.
When to See a Healthcare Provider
While many people successfully manage plantar fasciitis with conservative measures, you should consult a healthcare provider if you experience:
- Severe pain that limits daily activities
- Pain that persists despite several weeks of home care
- Numbness or tingling in the foot
- Significant swelling, redness, or warmth
- Fever along with foot pain
- Inability to bear weight on the affected foot
A healthcare professional can provide proper diagnosis, rule out other conditions, and recommend appropriate treatment options tailored to your specific situation.
Finding the Right Support for Your Feet
Living with plantar fasciitis can be challenging, but many people find significant relief through the right combination of supportive footwear, proper arch support, gentle stretching, and lifestyle modifications. Whether you're looking for arch supports for plantar fasciitis, the best insoles for your needs, or simply trying to understand how to help plantar fasciitis, remember that everyone's experience is different.
What works well for one person may not be ideal for another, which is why exploring different support options and working with healthcare providers to find the best approach for your individual needs is so important. Visit a Good Feet store to get personalized recommendations based on your unique foot structure and lifestyle needs.
With patience and the right support, many people successfully manage plantar fasciitis and return to their normal activities.
Remember, this information is educational in nature and not intended as medical advice. Always consult with qualified healthcare providers for diagnosis and treatment recommendations specific to your situation.
ASK THE EXPERTS
Concerns & Conditions
Learn more about different types of body pain and how arch supports can help
Discover a Life of Greater Comfort
Our Arch Supports Are Designed to Align Your Body from the Feet Up and Can Help Provide Relief from Pain and Discomfort.